Expanding Dragonfly Utilize Capabilities with GenAI
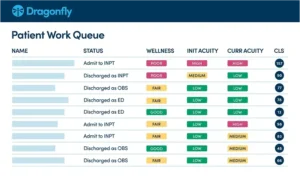
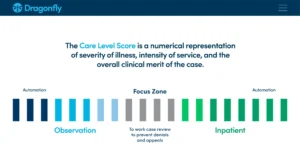
Utilize now includes powerful Generative AI capabilities that streamline the utilization review (UR) process, helping clinicians spend less time on documentation and more time on patient care. AI-guided initial reviews generate concise, comprehensive summaries directly within the UR workflow, saving nurses an average of 15 minutes per case. With our Human-in-the-Loop approach, UR nurses can easily review, refine, and finalize summaries ensuring accuracy, while accelerating approvals and reducing denials. The result is greater efficiency, improved coordination, and tools that truly make a difference in day-to-day clinical practice.
LEARN MORE