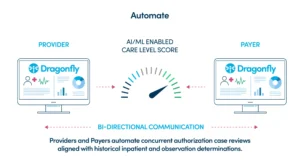
DRAGONFLY ALIGN FOR Health Plans, Provider Sponsored Health Plans, and More
A Seamless, 360° payer concurrent authorization solution across all teams
Make sure the right cases are seamlessly handled at the right time, by the right staff, with a shared framework for concurrent authorizations across providers and health plans that leverages AI and ML-driven predictive analytics focused on the true clinical merit of every case.
REQUEST A CONSULTATION